Chronic Fatigue Syndrome (CFS), or Myalgic Encephalomyelitis (ME), is a complex and debilitating medical condition characterized by extreme fatigue or exhaustion that does not improve with rest and is not caused by any underlying medical condition.CFS is a chronic condition that adversely affects a person’s capacity for everyday life and quality of life.
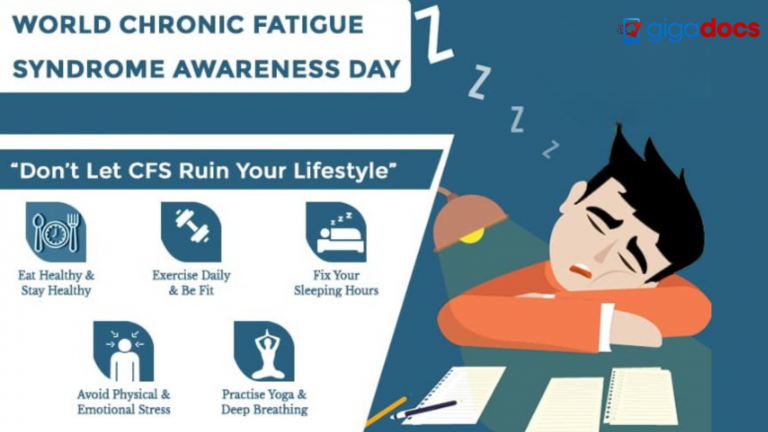
Chronic Fatigue and Immune Dysfunction Syndrome (CFIDS) is a common name for CFS in India. This Chronic Fatigue Syndrome International Awareness Day, let’s understand how common Chronic Fatigue Syndrome (CFS) is, why CFS is challenging to diagnose due to the variability in diagnostic criteria, and the underdiagnosis or misdiagnosis. However, CFS is estimated to affect between 0.2% and 2.5% of the population worldwide. Additionally, the symptoms of CFS/ME can overlap with other medical conditions, further complicating the diagnostic process.
Symptoms of Chronic Fatigue Syndrome (CFS)
Symptoms of Chronic Fatigue Syndrome (CFS) differ from person to person. The most prominent sign is persistent fatigue or exhaustion not relieved by rest. However, CFS is a complicated disorder, people may also have a variety of additional symptoms, such as:
- Fatigue: Overwhelming and persistent fatigue lasting at least six months and is not significantly improved by rest. This fatigue can interfere with one’s daily activities and harm one’s way of life.
- Sleep Problems: Disturbed or unrefreshing sleep is common in CFS. Individuals may have difficulty falling asleep, staying asleep, or experiencing non-restorative sleep, which means they wake up feeling tired or unrefreshed.
- Cognitive Difficulties: Many people with CFS experience difficulties with concentration, memory, and cognitive function. This is often called “brain fog” and can manifest as problems with thinking, processing information, and finding the right words.
- Muscle and Joint Pain: Widespread muscle and joint pain, sometimes described as myalgia and arthralgia, are frequently reported in CFS. The pain can be persistent and may fluctuate in intensity.
- Headaches: Recurrent headaches, including tension-type headaches and migraines, are common among individuals with CFS.
- Sore Throat and Tender Lymph Nodes: Some individuals with CFS may have a persistent or recurring sore throat. Additionally, the lymph nodes in the neck or armpits may become tender or swollen.
- Digestive Loss: Gastrointestinal symptoms such as bloating, nausea, irritable bowel syndrome (IBS), and food intolerances can occur in individuals with CFS.
- Sensitivity to Sensory Input: Individuals with CFS may be more sensitive to light, noise, odors, or certain foods, exacerbating their symptoms.
CFS is a complex and multi-systemic condition, and individual symptoms can vary. Individual symptoms of CFS, a complex and multisystemic illness, might differ. Furthermore, the symptoms mentioned above may also be present in other medical problems, making a diagnosis difficult.
How is Chronic Fatigue Syndrome caused?
It is still unclear what exactly causes Chronic Fatigue Syndrome (CFS). Genetic, immunological, environmental, and psychological variables contribute to the illness. Here are a few possible causes:
- Viral Infections: Some studies have suggested that viral infections, such as Epstein-Barr virus (EBV), human herpesvirus 6 (HHV-6), and others, may trigger or contribute to the development of CFS in some individuals.
- Immune System Dysfunction: Abnormalities in the immune system have been observed in individuals with CFS. It is believed that immune system dysfunction, including impaired response to infections, and chronic inflammation, may play a role in developing CFS symptoms.
- Genetic Predisposition: CFS may have a genetic component; these genetic factors could influence susceptibility to CFS or affect the functioning of the immune system and other physiological processes.
- Hormonal Imbalances: Some researchers have proposed that disruptions in the hypothalamic-pituitary-adrenal (HPA) axis, which regulates the body’s response to stress, may contribute to CFS. This can lead to abnormalities in the production and regulation of hormones, such as cortisol and other stress-related hormones.
- Environmental Triggers: Various environmental factors, including exposure to toxins, certain chemicals, or pollutants, have been suggested as potential triggers for CFS in susceptible individuals.
- Psychological Factors: While CFS is not primarily a psychological condition, psychological factors such as stress, trauma, and mood disorders may influence the onset or exacerbation of symptoms in some individuals.
Research in the field of CFS is ongoing, and the understanding of its underlying causes continues to evolve. Given the complexity of the condition, multiple factors interact to contribute to the development of CFS in different individuals.
How does Chronic Fatigue Syndrome affect other diseases?
Chronic Fatigue Syndrome (CFS) can impact other diseases or conditions in various ways. Here are a few examples:
- Co-occurrence of Other Conditions: It is not uncommon for individuals with CFS to have other medical conditions alongside it. These conditions can include fibromyalgia, irritable bowel syndrome (IBS), migraines, autoimmune disorders, and mood disorders such as depression and anxiety. CFS can complicate managing and treating these coexisting conditions, as symptoms can overlap and interact.
- Misdiagnosis and Delayed Diagnosis: CFS is a complex and often misunderstood condition. Its symptoms can mimic those of other medical conditions, leading to misdiagnosis or delayed diagnosis. This can result in inappropriate treatments or interventions for the individual’s underlying condition.
- Impaired Immune Function: CFS is associated with immune system dysfunction and individuals with CFS may be more susceptible to infections and other illnesses. This impaired immune function can make it more challenging for the body to fight off infections and recover from other diseases, potentially leading to longer recovery times and more severe symptoms in individuals with CFS.
- Exacerbation of Symptoms: Experiencing an acute illness or undergoing medical procedures known as post-exertional malaise (PEM) can worsen CFS symptoms in some individuals and can lead to prolonged fatigue.
- Challenges in Treatment: Treating other diseases or conditions in individuals with CFS may require special considerations. For example, medications commonly prescribed for certain conditions may have side effects that can exacerbate CFS symptoms. Additionally, chronic fatigue may affect an individual’s ability to follow complex treatment regimens or engage in intensive therapies for other life-threatening diseases.
Five things to know about Long Covid and chronic fatigue syndrome
Long Covid is a term used to describe the long-lasting effects of Covid-19 infection. It can affect individuals with mild, moderate, or severe initial Covid-19 symptoms. Here are the overlapping CFS factors that might be linked with Covid-
- Overlapping Symptoms: Long Covid and Chronic Fatigue Syndrome (CFS) are similar. Both conditions can involve persistent fatigue, brain fog, muscle and joint pain, sleep disturbances, and post-exertional malaise.
- Different Triggers: CFS can have various triggers, including viral infections, but it can also develop without a clear viral trigger. It’s important to note that not all individuals with Long Covid will develop CFS, and not all cases of CFS are preceded by a viral infection. Both these deadly infections can thus have different triggers.
- Impact on Daily Life: Long Covid and CFS can significantly impact an individual’s daily life and quality of life. Fatigue, cognitive challenges, and other symptoms can make it challenging to perform daily activities, including work, school, and social engagements. It’s essential to seek appropriate medical support and lifestyle adjustments to manage symptoms and improve well-being.
- Individual Variability: Both Long Covid and CFS can vary widely from person to person. The severity and duration of symptoms can differ, and the impact on daily functioning can vary greatly. Each individual’s experience with these conditions is unique, and personalized management plans are crucial. This explains why working with healthcare professionals to develop an individualized approach to symptom management is important.
- Long Covid and CFS are complex conditions requiring further research, clinical understanding, ongoing medical follow-up, symptom management, and a multidisciplinary approach involving healthcare professionals, support groups, and patient organizations.
How does Chronic Fatigue Syndrome affect kids?
Chronic Fatigue Syndrome (CFS) can affect children and adolescents, although it may be underdiagnosed or misdiagnosed in this age group.
The impact of CFS on children can be significant and affect several aspects of their lives, including physical health, education, social activities, and emotional well-being. Here are some ways CFS can affect kids:
- Fatigue and Energy Levels: Fatigue is a hallmark symptom of CFS and children with CFS experience persistent and debilitating fatigue that is not relieved by rest. This fatigue can significantly impact their energy levels, making it challenging to participate in daily activities, attend school regularly, and engage in physical activities or sports.
- Impaired Cognitive Function: Children with CFS may experience cognitive difficulties, including problems with concentration, memory, and information processing. This can affect their ability to focus on schoolwork, learn new concepts, and perform academically at their potential.
- School Attendance and Performance: CFS can result in significant school absenteeism, as children may struggle to attend classes consistently due to fatigue, pain, and other symptoms. Reduced school attendance may also lead to challenges in completing assignments, keeping up with school schedules, and engaging in extracurricular activities.
- Social Isolation: CFS can lead to social isolation for children. The limitations imposed by the condition, such as reduced energy levels and the need for rest, may prevent them from participating in social activities, spending time with friends, and attending social events. This isolation can negatively impact their emotional well-being and contribute to feelings of loneliness and frustration.
- Emotional Well-being: Living with a chronic illness like CFS can have emotional implications for children. They may experience frustration, sadness, and anxiety due to their physical limitations, social restrictions, and challenges in managing their condition. Emotional support, counseling, and involvement in support groups or peer communities can play a vital role in helping children cope with these emotional aspects.
Children with CFS need appropriate medical care, including a proper diagnosis and management plan. Dear parents, we advise you to download the Gigadocs app for medical treatments, cognitive behavioral therapy (CBT), and constant support from healthcare professionals.
How Does Chronic Fatigue Syndrome Affect the Male and Female Population?
Chronic Fatigue Syndrome (CFS) can affect both men and women, but some differences may exist. Here are some aspects to consider:
- Prevalence: CFS is more commonly reported in women compared to men. However, different factors, including social and cultural biases and the diagnosis of CFS among men and women, maybe the reason behind this difference.
- Symptoms: Studies suggest that men with CFS may be more likely to experience cognitive impairments and flu-like symptoms. Women may be more prone to report pain and fatigue as their primary symptoms.
- Social and Psychological Impact: CFS can have significant social and psychological effects on both men and women. It can disrupt personal relationships, employment, and social activities, leading to social isolation, frustration, and a decreased quality of life. The experience of living with a chronic illness like CFS can influence mental health and well-being, and both men and women may experience emotional challenges such as depression, anxiety, and stress.
When to see a doctor for Chronic Fatigue Syndrome (CFS)?
If you suspect that you have Chronic Fatigue Syndrome (CFS), it is advisable to consult a healthcare professional for a proper diagnosis when:
- Persistent fatigue: If you experience extreme fatigue that lasts at least six months or longer and is not relieved by rest or sleep.
- Impaired daily functioning: If the fatigue significantly interferes with your ability to engage in normal daily activities, including work, school, socializing, or household chores, it’s important to seek medical attention.
- Unexplained symptoms: Besides fatigue, CFS is often associated with other symptoms, such as muscle and joint pain, headaches, unrefreshing sleep, memory problems, sore throat, and tender lymph nodes. You should see a doctor if you experience these symptoms without a clear underlying cause.
Treatment for Chronic Fatigue Syndrome
Chronic Fatigue Syndrome (CFS) treatment focuses on managing symptoms, improving quality of life, and addressing any underlying factors contributing to the condition. There is no known cure for CFS; treatment involves a combination of strategies tailored to each individual’s needs. Here are some common approaches:
- Symptom management: Medications may be prescribed to alleviate specific symptoms such as pain, sleep disturbances, or depression.
- Cognitive behavioral therapy (CBT): CBT is a talk therapy that helps individuals change negative thoughts and behaviors. It can help manage stress, improve sleep habits, and address psychological factors that may exacerbate CFS symptoms.
- Graded exercise therapy (GET): Under the guidance of a healthcare professional, a structured exercise program can help gradually increase activity levels and improve physical functioning.
- Sleep management: Establishing healthy sleep habits and addressing sleep disorders can significantly improve CFS symptoms. Sleep hygiene practices and relaxation techniques can aid in improving sleep quality.
- Dietary adjustments: Some individuals with CFS may benefit from dietary modifications. Consulting with a healthcare professional or a registered dietitian for a balanced diet goes a long way toward identifying potential food sensitivities, nutritional deficiencies, or dietary triggers that may worsen symptoms.
Gigadoc’s telehealthcare app works closely with healthcare professionals and you to develop an individualized treatment plan. Download the Gigadocs app (link shared under) for customized treatment approaches based on the severity of CFS symptoms and overall health requirements.
Download the Gigadocs app from-
- IOS App – apple.co/2W2iG4V
- Android App – bit.ly/33AQoRC
To know more e-mail, at info@gigadocs.com